Paediatric Audiovestibular Medicine Service (Hearing)
The paediatric audiology service provides specialist care in identifying and managing children with a hearing impairment in Central and South Manchester.
The team’s aims are:
- to provide a high-quality and friendly service to children and their families who use our service
- to work collaboratively with other professionals such as community paediatricians, speech and language therapists, health visiting and school health teams as well as ear nose and throat and Manchester sensory teams.
The community paediatric audiology department has a well-established clinical team including one medical consultant in paediatric audiovestibular medicine, clinical scientists and paediatric audiologists working to provide an excellent service.
The service is available to anyone who has concerns with a child’s hearing or development or is known to have a hearing impairment. We assess and provide support for children of all developmental ages from birth to 18 years of age. Those children who require continuous management after the age of 18 will be transitioned to adult services through a dedicated specialist pathway. We ensure children and families are always involved in their care planning and create individual management plans according to their needs.
Audiology Provision of Services include:-
- A range of hearing assessments for all children (0-18 years)
- Hearing aid fittings and verification using digital hearing aids and follow-ups for children diagnosed with a hearing loss
- Hearing aid repair and maintenance service
- Tinnitus and Hyperacusis assessment and management
- Auditory Processing Disorder (APD) assessment and management
- Audiology input the Manchester hub of the North West, North Wales, and Isle of Man cleft palate network (for children diagnosed with cleft lip and/or palate)
- Transitioning service to Adult audiology
- Vestibular assessment and management
- Aetiological investigations for children diagnosed with permanent hearing loss undertaken by the consultant in paediatric Audiovestibular medicine
- Clinical services for other trusts in the field of audiology
There are many ways you are able to arrange an appointment with us. These include:
- Self-referrals
- GP referral
- Health visitor referral
- Any other specialist referral (i.e. Speech and language therapy, community paediatrician etc.)
- Referrals from Newborn hearing screening
Referrals into audiology are triaged by the consultant, who has a clinical responsibility for the central and south of Manchester. Patients are triaged as to their complexity and are aligned with the skills of the various audiology staff members with the aim to provide appropriate care with minimum delay. Once the referral has been accepted we will contact you to book an appointment. You will be sent an appointment letter which may have a questionnaire alongside it. We advise to fill it in and bring it with you to the appointment.
The service is available for children registered with a GP in Central and South Manchester.
You can refer to our service by using the Emis internal referral system. Alternatively, you can make a referral by using our email accounts:
mft.communityaudiology@nhs.net
Community.AudiologyTeam@mft.nhs.uk
For children registered with a GP in North Manchester, please send the referral to the following email address: Audiology.NMGH@mft.nhs.uk
Contact Details:
The Audiology service operates from various sites in the community. We aim to offer an appointment at the clinic site closest to you depending on the type of service required for your child.
Audiology Administration team
Paediatric Audiology Department
Moss Side Health Centre
Monton Street
Moss Side
M14 4GP
Phone: 0161 232 4214/4215
Email: mft.communityaudiology@nhs.net / community.audiologyteam@mft.nhs.uk
Text: 07870 986 972
Opening hours
Monday to Friday, 8:30am to 4:30pm
Excluding Bank Holidays.
Please note: Our phone lines are currently open between 9:30 – 3pm until further notice.
Using the contact information above you can leave a message, text us or email us at any time.
Brownley Green Health Centre
Brownley Road,
Wythenshawe,
Manchester
M22 9UH
Available for: hearing assessment, hearing aid fittings, aetiology, balance assessment, auditory processing assessment and tinnitus hyperacusis assessment
Download directions here.
Burnage Health Centre
347 Burnage Lane,
Manchester
M19 1EW
Available for: hearing assessment, aetiology , and tinnitus hyperacusis assessment
Download directions here.
Longsight Health Centre
526 – 528 Stockport Road,
Manchester
M13 0RR
Available for: hearing assessment, aetiology, and tinnitus hyperacusis assessment
Download directions here.
Royal Manchester Children’s Hospital
Oxford Road,
Manchester
M13 9WL
Available for: hearing assessment, and tinnitus hyperacusis assessment
Download directions here.
Withington Community Hospital
Nell Lane,
Manchester
M20 2LR
Available for: hearing assessment, aetiology , balance assessment
Download directions here.
What can I expect to happen during my child's appointment?
Microsuction Patient Leaflet [PDF, 471kb]
Paediatric Audiology Clinic Patient Leaflet [Word doc 464kb]
The tests we will use to check your child's hearing
Depending on the age of your child they may be seen by either one or two clinicians.
During the appointment, we will take a thorough history about your child’s hearing and development. We will choose an appropriate method of testing your child’s hearing, based on their age, ability and interests. These will provide us with information in relation to hearing levels and the general health of your child’s ears. Results will be discussed at the end of the appointment.
Below is a table of types of test we may use during the appointment according to the child’s developmental age.
| Distraction Testing | Used from around 6-8 months (can be used up to 24 months). A variety of sounds using rattles, voice, chimes or warble sounds are made at various levels either to the right or left side of the child, out of their field of view. Here we assess the child’s ability to hear the sound and turn their head to locate it. |
| Visual Reinforcement Audiometry | Used from around 6-24 months. Sounds are presented through speakers either side of the child and in response to the child hearing and turning to locate the sound, a visual reward is presented in form of an illuminated toy or flashing light. Here we can assess more frequency specific information which is important for speech development. We can also obtain ear specific information if completed using headphones or small insert tips placed into the child’s ear. |
| Play Audiometry | Used from 20 months to 5 years old. It is important the child understands simple instructions and commands for this assessment. A game is played where the child is asked to perform an action in response to hearing the sound. This could be by placing a man in a boat, a peg on a board or stacking toys. The sound can be presented in various ways depending on their developmental age such as loudspeaker, headphones or insert tips. Sounds are presented at various frequencies and we determine the lowest level the child can hear at each frequency. |
| Puretone Audiometry | Used for school aged children. Sounds are presented through wearing headphones or insert tips. The child is asked to press a button or saying ‘yes’ in response to hearing sound. Sounds are presented at different frequency and intensity levels. The sound is first presented at a louder level and gradually reduced until the child stops responding. Results are plotted onto an audiogram. |
| Otoscopy | An otoscope is used to check the child’s ears |
| Tympanometry | A tympanometer is used to assess the middle ear. A small soft probe is inserted in the child’s ear which changes the air pressure in the ear causing the ear drum to move back and forth. It can help determine if the child has fluid behind their eardrum or any perforations. |
| Otoacoustic Emissions | This is similar to the test used for newborn hearing screening. A small probe tip is inserted into the child’s ear and sound is presented, the inner ears (outer hair cell) response to this sound known as ‘echo’ is measured by the same probe. This test can give an indication of any damage to these hair cells which affect hearing thresholds. |
| Auditory Brainstem Response | This is similar to the test used for babies who have failed their newborn hearing screening. A set of electrodes are placed behind the babies ears and forehead. A click or tone pip sound is presented at various intensities. The electrodes will measure wave activity created by the sound pathway from inner ear up to the brain via the auditory nerve. |
Information on Other Hearing Related Conditions
What is Tinnitus?
Tinnitus is the sensation of hearing a sound when there is no external source for that sound. In a minority of cases, the sound may have a physical source within the body, like the sound of a person’s pulse, but in most cases, the sound is generated spontaneously by the hearing pathway and/or brain. Everyone’s tinnitus is different. Many people hear a ringing sound, but others hear whistling, buzzing or crackling. The noise may be heard in one ear, in both ears, in the middle of the head or it may be difficult to pinpoint its exact location. The noise may be low, medium or high-pitched. The noise may be continuous or it may come and go. It can be quiet or very loud, or the volume may fluctuate.
What does it feel like to have Tinnitus?
The majority of children are not troubled by their tinnitus and it does not affect them in their everyday life. However, a small number of children can be very distressed by it. For some children, tinnitus can become very intrusive resulting in fear affecting sleep, concentration and hearing. Tinnitus may be most noticeable when it is quiet such as at bedtime or during the night. They may describe a feeling of fullness in the ear. You may notice your child displaying feelings of anger, frustration and fear.
What can help?
Information counselling
Whilst the experience of tinnitus is common, most children with tinnitus are not bothered by it, and a simple explanation and reassurance are all that is required.
Relaxation exercises
As tinnitus is exacerbated by heightened tension some simple breathing and relaxation exercises can help reduce stress and anxiety.
Sound therapy
Background noise can help to reduce the perception of tinnitus and if used at bedtime can help with sleep
If your child experiences difficulty concentrating in quiet environments (such as during exam times) background noise presented through ear-level noise generators can be helpful. The audiologist will be able to do an assessment and provide these devices for your child.
What next?
If your child is experiencing symptoms of Tinnitus and it is significantly impacting on your everyday lives please see your GP to get a referral to the children’s audiology department for a full assessment.
What is Hyperacusis?
Hyperacusis is an exaggerated or inappropriate response to sounds that are neither threatening nor uncomfortably loud to a typical person. Common sounds which children find troublesome include that of vacuum cleaners, children screaming or playing, hand dryers, emergency sirens and alarms. It can lead to avoidance of noisy places such as parties, the cinema, the playground, dining room and the school canteen or if they attend wanting to leave early. At school children may find it difficult to concentrate and may not like to go to school. Hyperacusis can occur on its own or as part of an underlying condition such as migraine, post-head injury syndrome, Lyme disease, autism, ADHD and Bell’s palsy.
What does it feel like to have Hyperacusis?
In noisy environments children with hyperacusis can be seen holding their hands over their ears to block out the sounds. Children may feel pain, they may startle or start to cry when there are loud sounds. It may make them angry, distressed or anxious. They may start to panic and try to get away from the sound. Their reaction to an uncomfortable sound may be made worse if they are in an environment where they expect to hear the sound. It can be a minor nuisance to some but a life-altering experience to others.
What can help?
Information counselling
Parents and children can be very reassured if they understand what hyperacusis is and why it occurs.
Auditory desensitization program
It involves the gradual introduction to sound using sound therapy over a period of time. This can be delivered using ear level noise generator devices which are like little hearing aids with earmoulds placed behind the ear delivering a low level background noise. Sound therapy can also be delivered in the free field using any device which can present sound such as an ipad, radio, mobile phone. The audiologist will assess your child and devise an auditory desensitization program for your child. Treatment in children can vary from 6 months to 18 months. This program can be very helpful in managing hyperacusis in majority of children
Relaxation exercises
Hyperacusis can be exacerbated by anxiety and, therefore, simple relaxation exercise such as breathing and imagery can help to reduce tension.
Are Ear Defenders/earmuffs helpful in managing Hyperacusis?
It is advised to reduce the use of these devices as they can be counterproductive. They may provide relief in the short term but in the longer term they may be counterproductive and exacerbate hyperacusis. When using ear defenders, as the environment becomes quieter the auditory system becomes confused by this lack of sound input. The auditory system therefore becomes more sensitive in a misguided attempt to find the missing sound resulting in increased sensitivity making hyperacusis even worse.
What next?
If your child is experiencing symptoms of Hyperacusis and it is significantly impacting on your everyday lives please see your GP to get a referral to the children’s audiology department for a full assessment.
What is Misophonia?
The literal definition of misophonia is hatred of sound but a person with misophonia does not simply hate all sound. People with misophonia have specific symptoms and triggers and are sensitive to only certain sounds and occasionally are sensitive to visual triggers as well. The age of onset will often be around 10-12 years of age. The “trigger” sounds which tend to be most difficult are connected with people such as eating and breathing, slurping and chewing. Other sounds such as nail biting, tapping and clicking can also result in negative emotions. The closer the sufferer is emotionally to the “trigger” person, the more offensive the sound tends to be.
What does it feel like to have Misophonia?
The reaction starts with the sound (or some aspect of the sound) and often develops to include actions associated with the sound. The reaction can range from moderate discomfort to acute annoyance or go all the way up to extreme rage. The trigger sound can create an overwhelming fight or flight response in the sufferer, so they experience a desire to do extreme violence to the maker of the sound, or to escape the vicinity of the sound at all costs. Family mealtimes can become very difficult and the sufferer will eat alone.
What can help?
Information counseling
It is very helpful for a young person’s friends and family to understand what Misophonia is and its effects on a person with this disorder. Once made aware, they may be more supportive.
Sound Therapy
Pleasant music or background noise through earphones or in the free field can be helpful in masking or distracting from the trigger sounds when they occur and may reduce the level of anger or anxiety that is experienced.
Relaxation exercises
Misophonia is exacerbated by tiredness and tension. If used effectively relaxation exercises can be used to reduce anxiety and promote calmness.
Sometimes a referral to the psychology service for cognitive behaviour therapy may be recommended.
What next?
If your child is experiencing symptoms of Misophonia and it is significantly impacting on your everyday lives please see your GP to get a referral to the children’s audiology department for a full assessment.
What is APD?
Auditory processing disorder affects the ability of the brain to understand and interpret sounds.
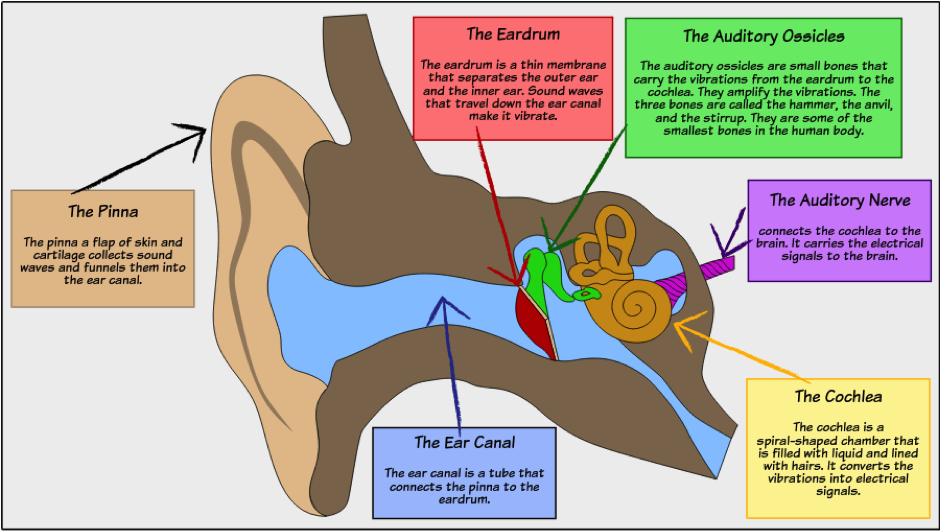
When a sound is made, sound waves enter the ear canal and pass through the middle and inner ear as normal. These sound waves are turned into electrical signals which then travel up to the brain via the auditory nerve. Once the sound arrives to the brain, there may be difficulties in processing the sound for example, understanding speech especially if there is background noise.
What are the symptoms?
APD can affect all ages and in different ways. It often starts in early childhood and becomes more noticeable when a child starts school. Hearing tests show normal hearing however these children can have:-
- Difficulties listening in noisy environments such as classrooms, playgrounds
- Difficulty understanding speech when more than two people talking and/or when there is poor signal quality such as through a phone and/or interpreting similar speech sounds. As a results, affecting ability to remember instructions/reading/spelling.
- Take longer to process auditory information therefore can take longer to respond
- APD can coexist with other conditions such as dyslexia, ADHD, language processing disorders which can worsen the symptoms
What are the causes of APD?
The cause of APD is unknown however; research is ongoing into this area. There could be a possible genetic component as often parents report similar struggles. In some cases it may be related to prolonged episodes of glue ear or recurrent ear infections affecting cells. APD can sometimes be linked to brain damage caused by an injury, tumour or meningitis. It can also be linked to traumatic births where there was a significant lack of oxygen to the brain.
How do you diagnose APD?
APD is diagnosed by using a series of tests and taking a detailed history. The test usually involves the child wearing headphones and responding back to what is being presented via repetition, pressing button or in other appropriate ways. APD tests depend on the age of the child and how much information we can get about their listening in different environments.
How is APD treated?
There is no cure for APD but strategies can be implemented to help manage symptoms of APD. The areas we focus on are:-
Changing the environment: explore different strategies to help with listening and understanding, provide advice sheets for schools
Use of technology: usage of personal FM systems or speaker systems in school to help with listening in background noise
For many children, APD can improve over time as children can incorporate coping strategies into their everyday life leading to a successful school and work life.
Further information
APD Support UK
APD Support UK are an organisation developed to provide extra support for children and adults suffering with APD
Website: https://apdsupportuk.yolasite.com
What is Noise Induced Hearing Loss (NIHL)?
NIHL is a hearing loss caused by sustained exposure to sounds loud enough to damage the tiny hair cells within our inner ear (cochlea). Many enjoyable sounds that we hear every day are at safe levels that don’t damage our hearing. However, sounds can be harmful when they are too loud-even for a short time-or when they are long-lasting, even if they are not quite as loud.
NIHL can be caused by being in environments with loud damaging levels of noise such as for example nightclubs, concerts, construction sites, factories, the orchestra and soldiers using firearms. Everyday activities can result in damaging levels of noise putting children at risk of NIHL. These include riding motorbikes, listening to music at high volumes through headsets or earbuds, being around noises at home for prolonged periods of time (for example lawnmowers and leaf blowers). The louder the sound, the faster it can damage your hearing.
What are the signs of NIHL
Hearing loss caused by noise can be temporary. For some people, hearing returns to its normal levels after 16 to 48 hours after exposure to loud noises. Recent research suggests, however, that there still may be long-term, permanent damage even if it isn’t noticeable /detectable immediately.
Hearing loss due to loud noises can also build over time, so you may not readily notice the signs. As hearing loss progresses, children might:
- Complain of ringing or buzzing in the ear –called tinnitus. Tinnitus may go away over time, but it can sometimes continue for a long time or throughout a person’s life.
- Say “What?” more often or ask others to repeat what they’ve said.
- Turn up the sound on the TV or other devices.
If your child experiences any of these signs regularly, you should get their hearing checked to determine if they have a hearing loss.
When is a sound too loud?
Sound is measured in units called decibels (dB). The decibel is used to describe sound based on what human ears can actually hear. The lower the number, the quieter the sound is for example a whisper is 30dBA, normal conversational speech is 65-75dBA and gunshot is 120dBA. Your hearing can be damaged by noise levels above 80dBA. The louder the sound, the shorter the amount of time it takes for a possible hearing loss to occur and this can vary from person to person. At 80dBA you can safely listen to the sound for 8 hours. Small changes above this level significantly reduce the safe listening exposure time. For example at 83dBA this is reduced by half to 4 hours and at 86dBA this is halved again to 2 hours so by 95dBA this only 15 minutes and by 110dBA an exposure of just 1 minute can damage hearing.
The noise thermometer below shows the range of loudness of everyday sounds and the exposure time that can cause hearing damage
Noise Thermometer
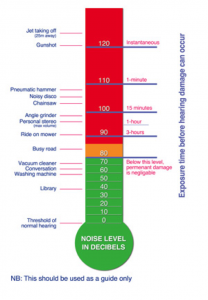
For example, a gunshot can cause hearing damage much more quickly than exposure to a power lawn mower at 90dBA.
How does noise damage hearing?
The following youtube video explains how the ear works. https://www.youtube.com/watch?v=eQEaiZ2j9oc
Too much noise too often and for too long can damage the tiny hair cells in your inner ear. Inner ear hair cells respond to sound by swaying to sound vibrations and send information to the brain through the nerve pathways. When they are damaged they cannot send signals to your brain. In humans, hair cell bundles cannot be fixed or replaced, so this damage leads to permanent hearing loss.
At first, the hearing loss is temporary, but if the noise exposure continues and the ear is not given time to recover, the hearing problem becomes permanent.
High-pitched sounds are affected in the early stages, so you can hear people speaking, but it may be difficult to make out all the words. More exposure to loud noise gradually makes the problem worse.
How to prevent noise-induced hearing loss
- Lower the volume. Always listen at safe levels. Sounds below 80 dBA are generally considered safe even when listening for long periods of time.
- Move away from the noise. Sounds get quieter as you get farther away from the source.
- Wear hearing protectors, such as earplugs or earmuffs in noisy places such as concerts where levels are likely to exceed 80dBA
- Do not stand too close to speakers or other source of loud noise
- Let your hearing get back to normal between noisy activities.
- Do not go to noisy places too often!
- Measure the sound around you to check if it is too loud and when to use ear protection? Look for a free sound level meter app for your smartphone. NIOSH noise measurement app is free to download.
Have a discussion with your child about listening safely with personal music players.
- Choose headphones that block out the sound around you. If over-the-ear or in-the-ear headphones have a good seal, it is less likely they will turn up the volume to drown out other sounds. It is important to be careful and remember that when moving around while listening to music with headphones or earbuds, they need to stay safe and hear important sounds around them such as approaching cars, trains, bicycles, and other people.
- Try to use headphones or earbuds for only one hour a day.
- If listening to music with headphones or earbuds for 1½ hours or less per day, to set their device to play at no higher than 80 percent of the maximum volume.
- If listening to music with headphones or earbuds for more than 1½ hours per day, to set their device to play at no more than 60 percent of the maximum volume.
- Ears need a rest: to take regular breaks from their headphones or earbuds.
- Don’t listen with just one earbud. It’s harder to hear the music and they might be tempted to turn up the volume, putting that one ear at serious risk.
- Watch this video together which demonstrates to children very simply how the hair cells are damaged on exposure to loud sounds. https://www.youtube.com/watch?v=xE7FwQUV1v8
Links for further information
Information on ear plugs
Information on NIHL
Additional information
Who needs to attend the appointment?
It is advised to bring only the child who the appointment is for with a parent/carer. This is to try and ensure a quieter environment and to minimise distractions during testing. If you require an interpreter for the appointment please let us know by contacting the administration team.
Should I still bring my child if they’re not feeling well?
If your child is unwell on the day of the appointment, give us a call to rearrange your appointment. It may be best to do this so the child is well rested for their assessment and will enable us to obtain more reliable results on a day they’re feeling better.
How do I cancel or rearrange an appointment
You can do this by phoning/emailing/texting us at our main Office
Moss Side Health Centre, Monton Street, Moss Side M14 4GP
Paediatric Audiology: 0161 232 4214/4215
Text: 07870 986 972
Email: mft.communityaudiology@nhs.net
How can I get my child ready for these tests?
You can show your child this leaflet to help them get ready to see us – leaflet coming soon.
You could also try:-
- Practicing using headphones at home. Your child could watch their favourite programme or listen to music whilst wearing headphones. This can help them get use to the sensation.
- Depending on their developmental age (from about 2.5 years) you could practice waiting skills for example ‘ready, steady and go’
What if my child does not cooperate?
If your child does not cooperate during the appointment, we can arrange another appointment in one of our specialised clinics where we can arrange for longer appointment times. It may sometimes take a few visits for us to establish hearing levels in young children or in those with special needs.
What happens if a hearing loss is detected?
Most children can be discharged with normal hearing. If a hearing loss has been picked up on the day of the assessment, we would first need to determine the nature of the hearing loss i.e. permanent or temporary and then discuss management options. We will provide you with support and advice on things that are best for your child.
What does a temporary hearing loss mean?
A temporary hearing loss usually suggests that the inner ear and the nerves that carry sound up to the brain are working well but that there is a problem with either the middle or outer ear. The most common causes amongst children for a temporary hearing loss is either a fluid build-up behind the eardrums as a result of a previous cold or infection, or possibly occluding wax. The fluid build-up is also referred to as ‘glue ear’. Management options for glue ear include waiting for this to resolve on its own (as it does in a number of cases), temporary hearing aids, and referrals to the ear, nose and throat department (for example for grommet surgery). The following link will discuss in more detail about glue ear and what to do when this is present.
https://www.nhs.uk/conditions/glue-ear/
What does a Permanent hearing loss mean?
The most common type of permanent hearing loss is referred to as a sensorineural hearing loss. This indicates damage to the hair cells in the inner ear or damage to the nerve that carries the sound to the brain. During the appointment if a hearing loss has been diagnosed, the severity of the loss will also be discussed alongside management options. We work with other services to ensure the best help for your child as efficiently as possible. Any help and support will be provided. We may also refer you to the aetiology clinic to try and obtain some more information relating to possible causes of the permanent hearing loss if not already known.
Is it normal to have ear wax?
Having a reasonable amount of ear wax (or cerumen) is healthy for your ears. Ear wax helps to keep debris, dirt and other things from entering the ear canal. Human ears are self-cleaning and so the wax inside the ears will eventually make its way out. However, wax can become a problem if it builds up over time and blocks the ear canal. This means the sound is not passing through the ear canal and going through the pathway as easily as it once did and thus sounds must be made louder for it to pass through. If this is the case when we see your child during an appointment, we can arrange for the wax to be removed. In the meantime, olive oil drops can be used to soften the wax and help make its way out.
If your child has been diagnosed with a hearing loss they may be suitable for hearing aids. This will be assessed by your audiologist and options will be discussed with you and your child. We use Phonak as our leading supplier for NHS digital hearing aids. The hearing aid will be programmed to match to your child’s level of hearing loss.
We supply:
Behind the ear (BTE) aids – used for children with temporary and permanent hearing loss
CROS aids – used for children with unilateral/single sided deafness
Bone conduction aids – used for children with conductive hearing loss or where BTE aid was not suitable (due to malformation of ear, recurrent ear infections)
For BTE aids your child will be able to choose from a range of colour options.
Hearing aid care and maintenance resources
(we can have the videos either as links or can have front page of the video with title up)
Ear moulds
How to insert a hearing aid with ear mould
https://c2hearonline.com/custom_mould/insertion.html
How to replace tubing
https://www.youtube.com/watch?v=CVJeA4FEjhQ&feature=player_detailpage
How to trim tubing
How to clean the earmould
https://c2hearonline.com/custom_mould/hearing_aid_care.html
Slim tubes
How to insert a hearing aid with slim tube
https://c2hearonline.com/openfit/insertion.html
Battery safety Advice – safe use, storage and disposal of batteries
A national patient safety alert stated that all babies and children under five years of age must be fitted with hearing aids with secure battery compartments, due to the risk of being swallowed. This includes older children who live with younger children and babies.
Safe Use
- Ensure tamperproof compartment is securely fastening when hearing is in use
- When not in use hearing aid should be switched off and stored out of sight/reach of young babies/children. You should be given a hearing aid care and/or dry beaker
Storage
- Ensure batteries are stored safely out of babies/young children sight
- Keep your used batteries in its original packaging so that you know old batteries have not gone missing
- Do not store batteries around food items as they can be mistaken for sweets
- Do not store in medication boxes
Disposal
- Used batteries can be placed in battery recycling bins, which can be found in supermarkets, local recycling centre. You can also return your used batteries to the audiology clinic.
What to do with my child swallows a battery?
If your child swallows a battery seek immediate medical attention. Do not let them eat or drink until it has been determined if a battery is present by the hospital. Take the battery packaging with you and show the doctor
Children Hearing Services Working Group (CHSWG)
What is the CHSWG?
The children’s hearing services group (CHSWG) is made up of representatives from services supporting children with hearing impairment and their families. These include audiologists, newborn hearing screeners, teachers of the deaf and speech and language therapists, Manchester deaf centre as well as parents of children with hearing impairment. Their aim is to help continually improve quality of services provided and offer support/guidance for these children. The group meets three times a year to share actions, experiences and ideas.
Manchester Sensory Support Service
The service provides support for children with hearing or vision impairments and their families. They work with nurseries and state funded schools to provide advice and training in order to improve a child’s educational achievement, communication skills, social and emotional wellbeing.
For further information visit:-
Useful Links
- NHS Hearing test for children – Overview of why it is important to have hearing checked and what to expect
https://www.nhs.uk/conditions/hearing-tests-children/ - National Deafness Society – The leading charity for deaf children who provide excellent support and information for children and their families
https://www.ndcs.org.uk/ - Manchester Deaf Centre – Manchester Deaf Centre is the largest organisation in Greater Manchester that provides support to a wide range of people with hearing loss
http://www.manchesterdeafcentre.com/ - C2 Hear Hearing well together -The C2Hear interactive multimedia videos improve the lives of new hearing-aid users
https://c2hearonline.com - Newborn Hearing Screening – Overview of the newborn hearing screening programme for babies and how it is completed
https://www.gov.uk/guidance/newborn-hearing-screening-programme-overview
Checklists for babies
– Making Sounds Checklist
– Reacting to Sounds Checklist
Phonak Listening room
Free, fun activities and resources to support the development of speech, language, and listening skills in people of all ages with a hearing loss – https://thelisteningroom.com/home
Page last reviewed: January 2023
Next review due: October 2023
